Pediatric Critical Care Medicine Fellowship
The goal of the Pediatric Critical Care Medicine fellowship training program at Ann & Robert H. Lurie Children's Hospital of Chicago and Northwestern University's Feinberg School of Medicine is to provide comprehensive training to pediatricians in the scientific and clinical practice of pediatric critical care medicine. This training includes those elements that typify an accomplished and well-rounded practitioner, including medical knowledge, clinical skills, research skills, humanistic qualities, professionalism and a commitment to scholarship and life-long learning. We match four to five fellows each year in this three-year fellowship program (total compliment of 13 fellows). Current fellows come from top programs across the country and have a wide range of backgrounds and interests within critical care.
MISSION: Development, evolution, and preservation of a thriving training program
VISION: An environment which facilitates the development of a critical care fellow towards a fulfilling and happy career, a composite of excellence in clinical care, contributions to the field, and propagation of practice, education, and advocacy for others.
VALUES:
- Continual Improvement and Curiosity
- Health Equity
- Safety across paradigms
- Multidirectional accountability
Video: meet Dr. Adrian Zurca, fellowship program director

Education
We approach the education of critical care fellows with a well-rounded curriculum. New fellows participate in an orientation curriculum that includes local and regional simulation-based “bootcamps” focusing on clinical skills, teamwork and communication. A comprehensive didactic curriculum is provided during weekly conferences. The content is guided by the Critical Care Subboard of the American Board of Pediatrics content outline and includes fundamental physiology and applications to the practice of critical care. Recurring conferences address administrative aspects of critical care practice, ethics, neurocritical care, cardiac critical care and case-based physiology. Fellow participate in critical review of their practice via quarterly morbidity and monthly mortality conferences. In addition, regular journal clubs and research updates by division members offer an opportunity to evaluate innovative therapies and examine proposed mechanisms of critical illness. An active simulation program through the kidSTAR simulation center provides realistic immersion in physiology and team dynamics. Fellows also participate in monthly board review sessions which focus on topics covered in the previous month’s didactics to allow for spaced-repetition in learning. Fellows also have the opportunity to learn in a small group setting from various critical care faculty in twice monthly “chief rounds” sessions.
Research
The goal of the research experience is to provide fellows with the foundation for academic achievement through active participation in hypothesis-driven research under the supervision of an experienced mentor. Through completion of a scholarly project, fellows will demonstrate a basic understanding of the components of the scientific process, including analyzing medical literature, designing and implementing a study, data analysis and writing a manuscript. Fellows participate in a research curriculum taught through didactics, workshops, works-in-progress and formal research presentations.
Current and past fellows have pursued clinical, translational and basic science research, covering diverse topics such as energy estimation in critically illness, long-term outcomes of PICU patients and their families, microbiome, pharmacokinetics, causes and outcomes of cardiac dysfunction and medical education. Fellows are expected to present their work at a national meeting during the third year of fellowship. The faculty in the Division of Critical Care have a variety of research interests, including bioinformatics, ethics, patient and family experience, innovation, post-ICU outcomes, palliative care and inflammation. They often serve as mentors to the fellows.
Clinical Experience
Our fellows care for patients in a 40-bed pediatric intensive care unit as well as a separate 44-bed pediatric cardiac care unit (CCU). The fellows are integral in the care of patients treated at Lurie Children's for a broad range of illnesses including level 1 traumas, solid organ and stem cell transplants, cardiothoracic surgery, otolaryngology and neurosurgery. Fellows develop the knowledge and leadership skills essential to becoming independent intensivists through clinical experiences such as direct patient care with multidisciplinary teams, directing medical control for the transport team and leading the code team. In addition to service time in the PICU and CICU, the fellows rotate in anesthesiology, the neurocritical care service and the interventional cardiac catheterization lab. Fellows are supervised in the PICU by a group of 18 critical care faculty members who provide 24/7 in-hospital coverage. In the CCU, fellows will work with faculty members who have training in both cardiology and critical care.
Clinical time is spread throughout the three years of fellowship training but is concentrated in the first and third years. The schedule is constructed to facilitate graduated autonomy and senior fellows work closely to supervise and support new fellows. Fellows do not take call during the week while on clinical service in the PICU to allow for continuity of patient care and team leadership. The night call schedule is designed to optimize continuity of research time during the second and third years of fellowship.
Requirements & Eligibility
Applicants to the fellowship program should be certified by the American Board of Pediatrics in general pediatrics or in the process of completing an ACGME-accredited pediatrics residency program that will allow them to be board-eligible prior to starting fellowship.
Application Process
Applicants must submit a CV, personal statement, three letters of recommendation, official medical school transcript and USMLE transcript. All documents should be transmitted through the ERAS system. Selection is completed through the NRMP fall pediatric subspecialty match. Fellowship interviews are conducted August to November of the year preceding the start of fellowship.
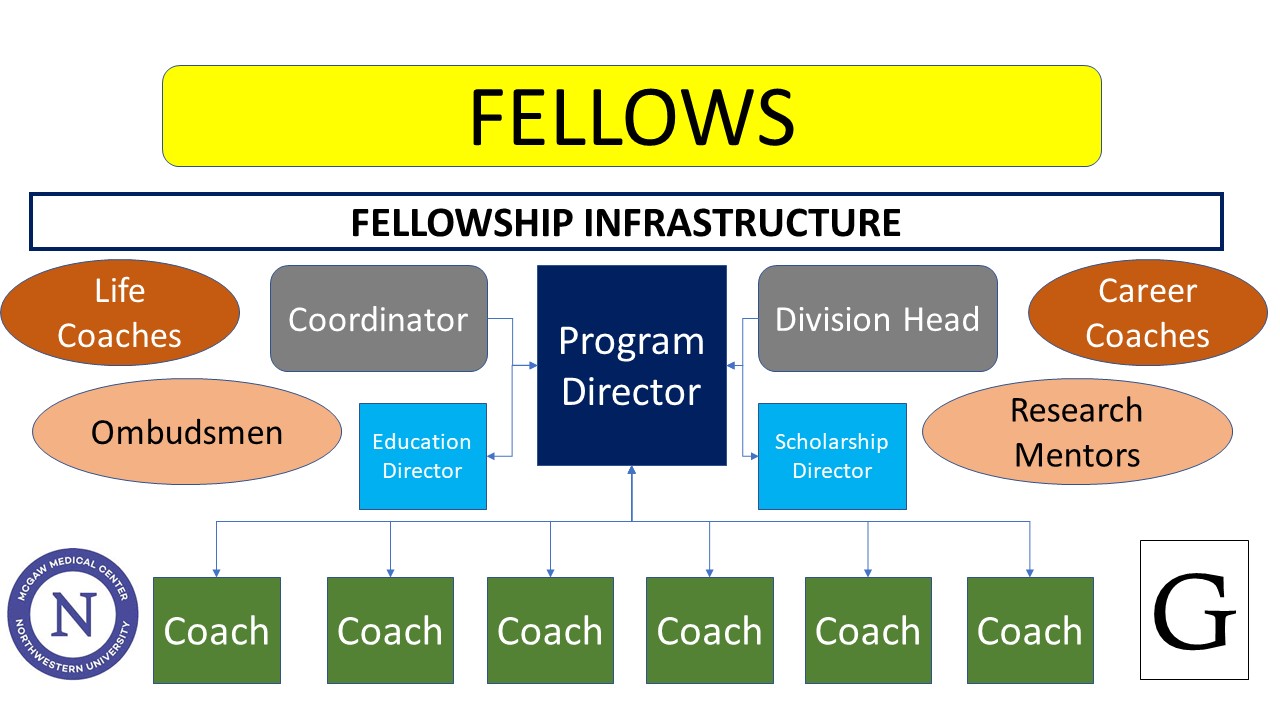
Key Personnel:
Program Director (Interim): Raj Basu, MD
Program Director: Adrian Zurca, MD
Scholarship Director: Conrad Epting, MD
Educational Director: Sue Hong, MD
Advocacy
Discover the many ways our faculty are impacting children's health beyond the hospital.
Global Health
Each year, as many as 20 third-year pediatric residents travel to Bugando Medical Center in Mwanza, Tanzania, to participate in an educational initiative that provides exposure to the management of complex pediatric diseases in a low-resource setting. Learn more about this extraordinary opportunity.
Why Northwestern?
 Housestaff training through McGaw Medical Center of Northwestern University provides diverse and challenging clinical experiences and world-class education located in the heart of the beautiful city of Chicago.
Housestaff training through McGaw Medical Center of Northwestern University provides diverse and challenging clinical experiences and world-class education located in the heart of the beautiful city of Chicago.
Watch Our Videos
Video Gallery
Meet Dr. Craig M. Smith, MD, Pediatric Critical Care / Neurocritical Care at Lurie Children's
Craig M. Smith, MD is a Pediatric Critical Care / Neurocritical Care Intensivist at Ann & Robert H. Lurie Children's Hospital of Chicago.
Meet Dr. Marcelo Malakooti, Pediatric Critical Care at Lurie Children's
Dr. Marcelo Malakooti is an attending physician in the Division of Critical Care (Pediatric Intensive Care Unit) at Ann & Robert H. Lurie Children's Hospital of Chicago.
Lefkofsky Family Pediatric Intensive Care Unit
See how the team in the Lefkofsky Family Pediatric Intensive Care Unit at Lurie Children's comes together to save the lives of the most critically-ill children.
Explore the Pediatric Intensive Care Unit
Meet Dr. Conrad Epting, Cardiac Intensivist, Heart Center at Lurie Children's
Dr. Conrad Epting, a cardiac intensivist in the Regenstein Cardiac Care Unit (CCU) at Ann & Robert H. Lurie Children's Hospital of Chicago. He specializes in both cardiac critical care and critical care (Pediatric Intensive Care Unity).
Contact Us
Adrian D. Zurca, MD
Fellowship Program Director, Pediatric Critical Care Medicine Fellowship
Critical Care
Conrad Epting, MD
Associate Program Director for Scholarship, Pediatric Critical Care Medicine Fellowship
Critical Care
Candace Mannarino, MD
Associate Program Director for Curriculum, Pediatric Critical Care Medicine Fellowship
Critical Care
Leah B. Davis-Burnett
Administrative Supervisor, Division of Critical Care Medicine
Critical Care
312.227.5359
Cathy Humikowski, MD
Associate Program Director for Wellness, Pediatric Critical Care Medicine Fellowship
Critical Care
More Information
Further program details, including the housestaff manual and a sample training contract, are available on the McGaw Medical Center of Northwestern University site.
Physician-Scientist Training & Resources
We offer a wide range of resources, mentorship opportunities and formal training programs to help our residents and fellows excel as physician-scientists. Explore all of the resources and hear from housestaff who are making research a major part of their career development plans.